The article has been reviewed by Dr. Au Hon Da, Kenneth, Specialist in Gastroenterology & Hepatology, St. Paul's Hospital
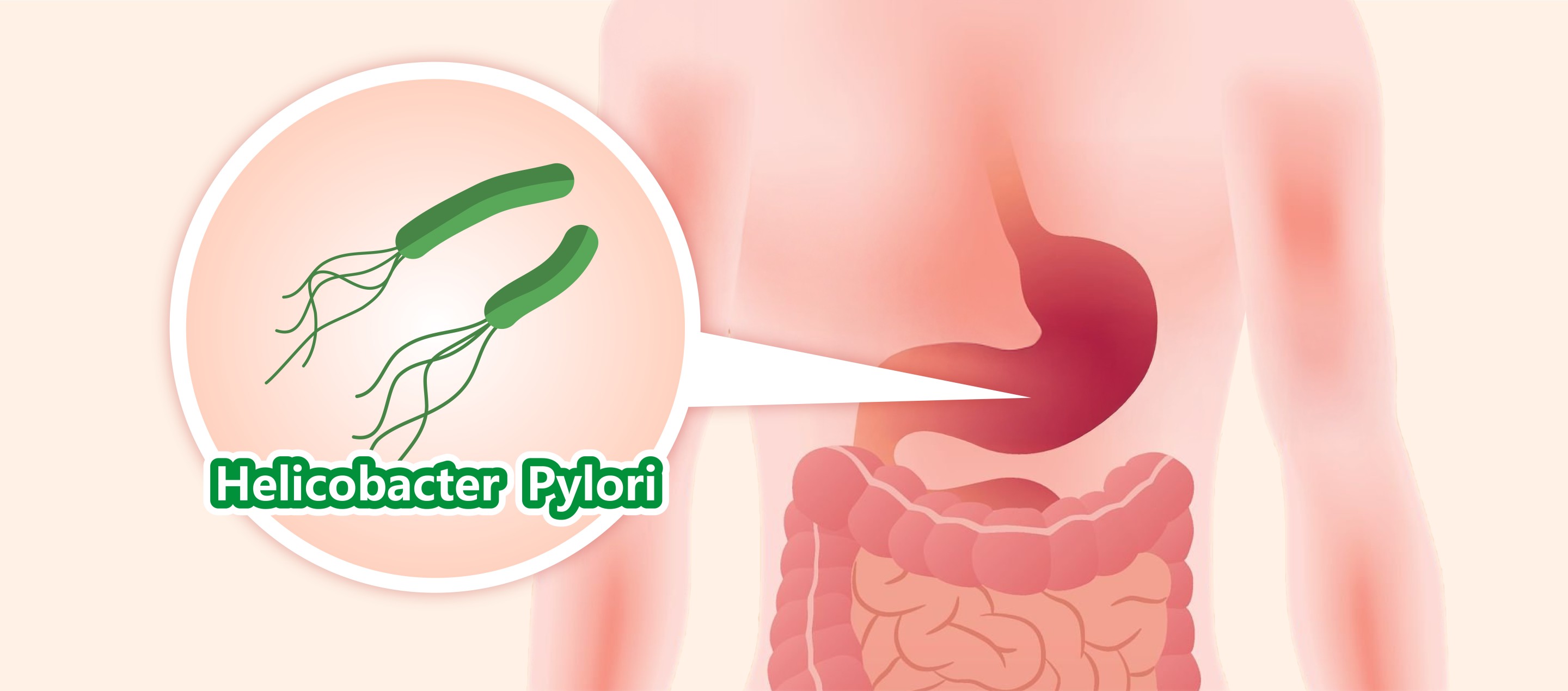

Helicobacter pylori (H. pylori) is a bacterium that resides in the stomach and duodenum, primarily living in the gastric mucosa or mucous cells. It can cause stomach discomfort, digestive system diseases, and even increase the risk of stomach cancer. Due to the lack of obvious symptoms in the early stages of infection, many people are unaware of their condition. This article will introduce the characteristics of H. pylori, symptoms of infection, transmission routes, diagnosis, and treatment methods, along with relevant preventive measures.
What is Helicobacter Pylori?
Helicobacter pylori is a spiral-shaped bacterium that can survive in acidic environments and affects stomach health. Infection with H. pylori can lead to gastritis, gastric ulcers, and is even associated with stomach cancer. This bacterium mainly spreads through saliva, fecal-oral routes, or contaminated food and water.
How Common is Helicobacter Pylori?
The infection rate of H. pylori is quite high worldwide. According to a study by the Chinese University of Hong Kong's Faculty of Medicine in 2017, over half of the population in Asia are carriers of H. pylori1. Some individuals may remain asymptomatic after infection but still have the potential to develop stomach diseases.
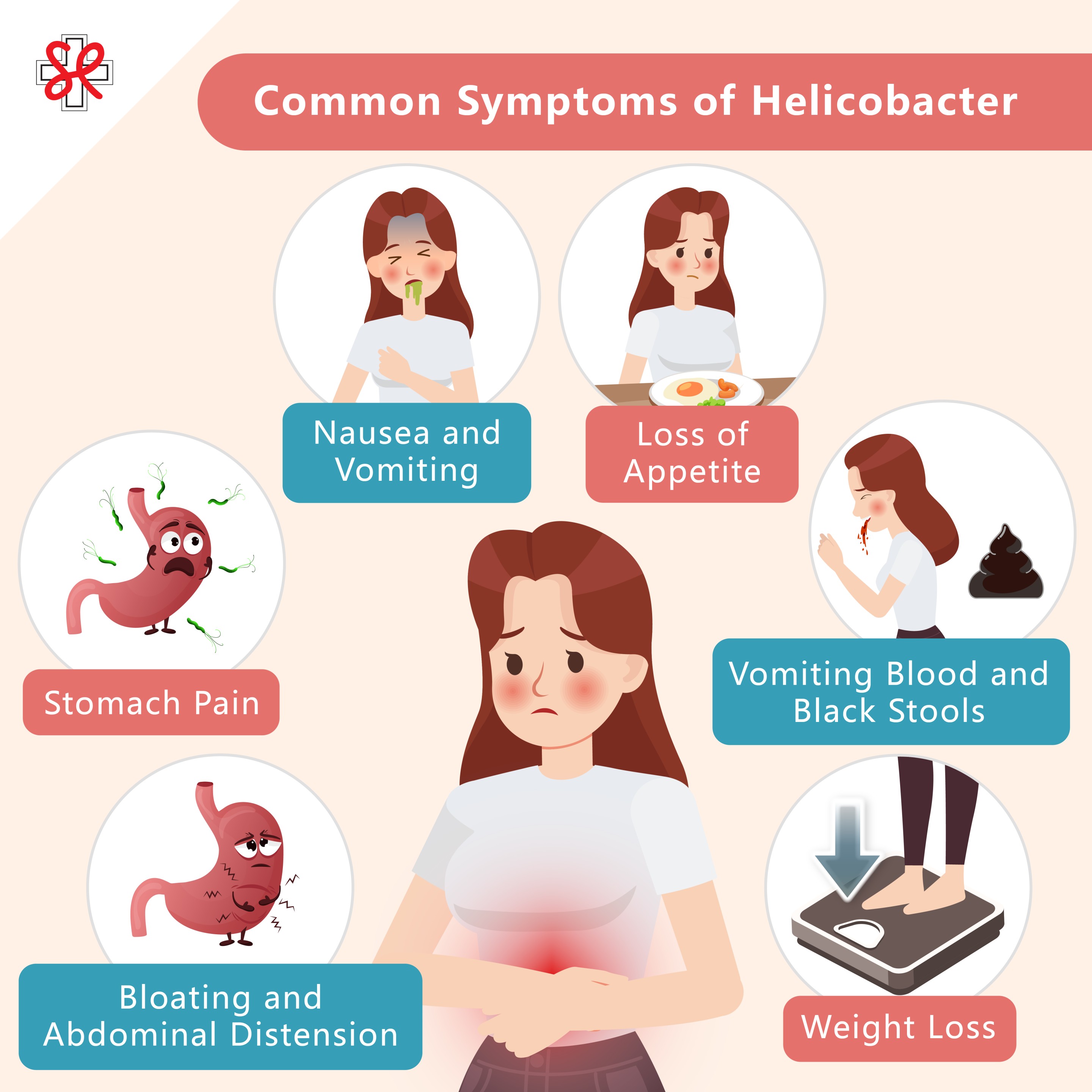
Common Symptoms of Helicobacter Pylori Infection
Most people infected with Helicobacter pylori may not exhibit any symptoms initially, but as the condition progresses, the following symptoms may arise:
( ![]() Click the image to enlarge )
Click the image to enlarge )
Bloating and Abdominal Distension
After an H. pylori infection, patients may experience bloating in the stomach or abdomen, often accompanied by a burning sensation, especially after eating. This symptom may be related to inflammation of the gastric mucosa, leading to weakened gastric motility, and is a common early symptom of H. pylori infection.
Stomach Pain
Stomach pain is one of the common symptoms of H. pylori infection, typically located in the upper abdomen. Discomfort may become more pronounced when the stomach is empty or at night. H. pylori neutralizes gastric acid by secreting urease, altering the local environment, while also stimulating increased gastric acid secretion, damaging the protective gastric mucosa and making the stomach wall more susceptible to acid injury, resulting in noticeable pain.
Nausea and Vomiting
Patients infected with H. pylori may experience persistent nausea and vomiting, particularly after meals. This is due to gastric inflammation irritating the gastric mucosa, triggering discomfort and the vomiting reflex.
Loss of Appetite
Patients may experience a reduced appetite or even a complete loss of desire to eat. This is often due to gastric inflammation causing discomfort, which affects the patient's willingness to eat.
Vomiting Blood and Black Stools
In more severe cases, patients may exhibit symptoms such as vomiting blood or passing black stools. This is usually caused by gastric ulcers or duodenal ulcers leading to ruptured gastric mucosa and subsequent bleeding.
Weight Loss
Some patients may experience weight loss due to loss of appetite, indigestion, or chronic bleeding.
Transmission Routes and Causes of Helicobacter Pylori Infection
Helicobacter pylori is primarily transmitted through the following methods:
- Fecal-Oral Transmission: Consuming contaminated food or water can introduce the bacteria into the stomach, leading to infection.
- Oral-Oral Transmission: The bacteria can spread between individuals through shared utensils, kissing, or sharing food.
- Iatrogenic Transmission: Incomplete disinfection of instruments during endoscopy or treatment procedures can lead to cross-infection.
- Environmental Hygiene Impact: Areas with poor personal and public hygiene conditions typically have higher rates of H. pylori infection.
Risk Factors for Helicobacter Pylori Infection
Below groups of people are at a higher risk of H. pylori infection:
- Crowded Living Conditions: The likelihood of bacterial transmission is higher in densely populated environments.
- Poor Sanitation: Lack of clean drinking water and good hygiene practices can increase the risk of infection.
- Living with Infected Individuals: Family members living with an infected person are more susceptible to transmission.
- Residing in High-Infection Areas: Infection rates are higher in certain regions, such as Africa (79%), Latin America and the Caribbean (63%), and Asia (55%), increasing the likelihood of infection among residents. 1
- Long-Term Poor Dietary Habits: A diet high in processed foods and salt can negatively impact stomach health and elevate infection risk.
- Chronic Use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): These medications can affect the stomach's mucosal defense, increasing the risk of infection.
Maintaining good personal hygiene, healthy eating habits, and avoiding sharing utensils with infected individuals can help reduce the risk of H. pylori infection.
Possible Complications
If left untreated, Helicobacter pylori infection may lead to the following complications:
Gastric Mucosal Inflammation
H. pylori can cause chronic gastritis, affecting the health of the gastric mucosa and resulting in stomach discomfort and pain.
Gastric and Duodenal Ulcers
The bacteria can damage the protective mucosa of the stomach and duodenum, leading to gastric acid eroding the stomach wall and forming ulcers, which can cause persistent abdominal pain.
Stomach Cancer
Long-term infection with H. pylori increases the risk of stomach cancer, particularly in patients with chronic gastritis and those with a family history of gastric cancer.
How to Diagnose Helicobacter Pylori Infection
There are several methods to detect H. pylori infection, including:
Blood Tests
Testing for antibodies to H. pylori in the blood can indicate whether a patient has ever been infected with the bacteria. However, this method has lower accuracy and is typically not used as a primary diagnostic tool, serving only for preliminary screening.
H. Pylori Breath Test / Carbon-13 Urea Breath Test
After swallowing a medication containing the carbon-13 isotope, if H. pylori is present in the stomach, the bacteria will break down the medication and release specific gases. This can be detected through breath analysis, making it a non-invasive and accurate test.
Stool Tests
Testing for H. pylori antigens in stool can determine if there is an infection. The process involves collecting a stool sample and sending it to a laboratory for analysis, commonly using enzyme-linked immunosorbent assay (ELISA) to confirm the presence of H. pylori antigens. This test is less accurate than breath tests.
Oesophagogastroduodenoscopy (OGD) and Biopsy
Oesophagogastroduodenoscopy (OGD) is an important tool for diagnosing upper gastrointestinal diseases and testing for H. pylori infection. This safe and accurate procedure allows doctors to directly observe the esophageal, gastric, and duodenal mucosa in real-time, assessing for ulcers, tumors, or inflammation. A biopsy can be performed during the procedure. Additional therapeutic procedures can also be performed at the same time. This method not only confirms the presence of H. pylori but also evaluates the extent of gastric mucosal damage. Based on the degree of damage, the doctor may choose to address issues immediately or arrange for follow-up treatment. The examination is usually conducted under local anesthesia or sedation. A flexible endoscope, about 0.9 to 1.2 cm in diameter, is inserted through the mouth into the digestive tract, taking approximately 5 to 20 minutes. Patients typically can return home the same day. Before the procedure, the doctor may spray a local anesthetic in the throat and, if necessary, administer a sedative. During the examination, patients will be connected to monitoring equipment to closely observe vital signs.
If you would like to make further inquiries, you may book an appointment at the Integrated Specialist Centre of St. Paul's Hospital. If relevant symptoms are present, the doctor will arrange for further examination at the Endoscopy Centre.
Treatment Methods
Treating Helicobacter pylori (H. pylori) infection typically requires a combination of multiple medications. Common treatment regimens include the following categories:
Proton Pump Inhibitors (PPIs)
Proton pump inhibitors such as omeprazole, pantoprazole, esomeprazole, and lansoprazole effectively suppress gastric acid secretion, relieve stomach discomfort, and promote the healing of the gastric mucosa.
Antibiotic Combinations
Commonly used antibiotics include:
- Amoxicillin: Disrupts the bacterial cell wall structure.
- Clarithromycin: Blocks bacterial protein synthesis.
- Metronidazole: Interferes with bacterial DNA synthesis.
- Tetracycline: Inhibits bacterial protein synthesis.
These antibiotics target the metabolic weaknesses of H. pylori, using different mechanisms to block bacterial survival. If a patient is allergic to penicillin-based antibiotics, metronidazole is usually used as a substitute for amoxicillin.
Histamine (H-2) Blockers
Medications such as ranitidine and famotidine can block gastric acid secretion, reducing gastric mucosal irritation and promoting ulcer healing.
Bismuth Subcitrate
Bismuth subcitrate is often used in combination with antibiotics to protect the gastric mucosa, decrease gastric acid erosion on the stomach wall, and inhibit H. pylori.
Mucosal Protectants
Sucralfate is a type of gastric medication that forms a protective layer on the gastric mucosa, reducing acid erosion and promoting ulcer healing.
Precautions
During treatment, it is crucial to strictly follow the doctor's instructions regarding medication timing. Even if symptoms improve, do not stop taking medication without consulting a doctor. If side effects (such as persistent diarrhea or rashes) occur during treatment, or if discomfort persists after treatment, seek immediate medical advice from Specialists in Gastroenterology & Hepatology to adjust the treatment plan or conduct further examinations.
Prevention Methods
To prevent H. pylori infection, maintaining good hygiene practices and a healthy lifestyle is essential. Here are some specific preventive measures:
1. Maintain Good Personal Hygiene
Develop the habit of thoroughly washing hands with soap and water before and after meals and after using the restroom to avoid contact with contaminated food and water, reducing the risk of H. pylori infection. Additionally, use separate utensils when dining to minimize the chance of oral transmission, further protecting your health and that of your family.
2. Ensure Dietary Hygiene
To ensure dietary hygiene, avoid consuming undercooked or contaminated foods, especially seafood and meat. It is advisable to drink treated clean water and avoid unpurified raw water to reduce the risk of bacterial infections. Additionally, limit the intake of processed foods and high-salt items, as these can increase the burden on the stomach and affect mucosal health. Instead, focus on consuming fresh vegetables and fruits to maintain a balanced diet and support good digestive system function.
3. Regular Health Checkups
Individuals with symptoms of stomach discomfort (such as stomach pain, bloating, or loss of appetite) or a family history of stomach cancer should undergo regular endoscopic examinations or other relevant tests to facilitate early detection and treatment of H. pylori infection.
Frequently Asked Questions
How Can I Know If I am Infected with Helicobacter Pylori?
If you experience symptoms such as bloating, stomach pain, nausea, or loss of appetite, it is advisable to seek medical attention for testing. Common diagnostic methods include breath tests, stool antigen tests, and endoscopy.
Is Helicobacter Pylori Contagious?
Yes, H. pylori mainly spreads through the fecal-oral route, such as through contact with contaminated food or water, as well as close contact with infected individuals.
Do I Need to Avoid Certain Foods If Infected with Helicobacter Pylori?
After being infected with H. pylori, it is recommended to avoid high-salt, high-acid, spicy, and irritating foods, as well as high-fat and fried foods. These can exacerbate stomach discomfort.
Can Helicobacter Pylori Cause Reinfection?
While most patients can eradicate H. pylori after treatment, there is still a possibility of reinfection in conditions of poor hygiene or close contact with infected individuals.
Will Helicobacter Pylori Heal on Its Own?
H. pylori infection typically does not resolve on its own. Without treatment, the infection may persist and could lead to more serious gastric conditions. Therefore, medication is necessary to eradicate the infection.
Reference:
- Nguyen LH, et al. The Changing Epidemiology of Helicobacter pylori Infection. Gastroenterology 2017;153:420–429.