The article has been reviewed by Dr. Wong Chung Ting, Martin, Specialist in Orthopaedics & Traumatology, St. Paul's Hospital


A herniated disc is a common spinal condition that can cause symptoms such as lower back pain, sciatica, and limb numbness, severely impacting the quality of daily life. This article will explore the causes, symptoms, diagnostic methods, and treatment options for herniated discs, allowing you to gain a comprehensive understanding of this condition and develop effective management and prevention strategies to improve your quality of life.
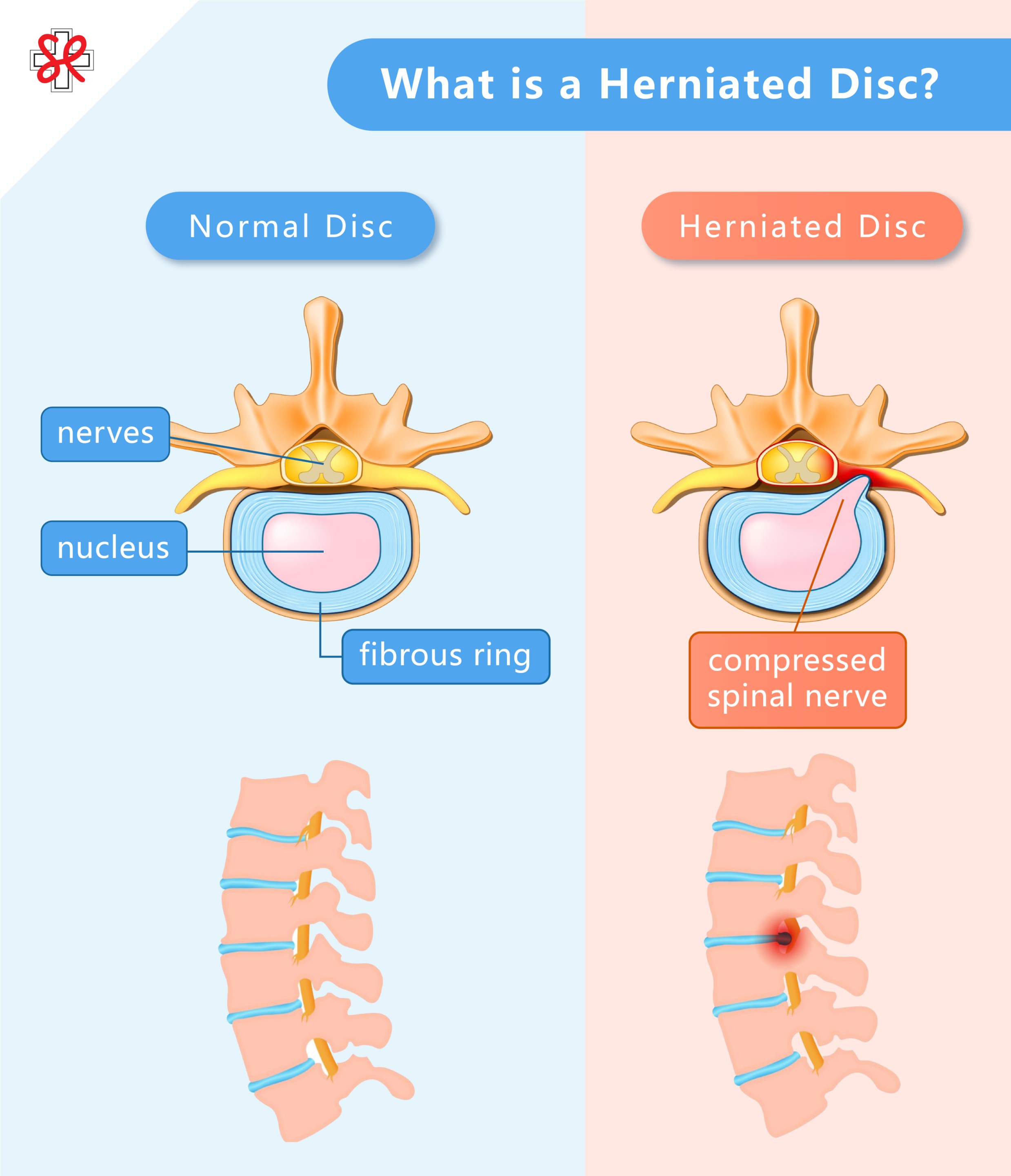
What is a Herniated Disc?
( ![]() Click the image to enlarge )
Click the image to enlarge )
A herniated disc, also known as a disc bulge or slip, is a common spinal issue often found in the lumbar and cervical regions. Herniated discs in the lumbar spine are most prevalent in the lower back, potentially causing lower back pain, sciatica, or leg numbness. Cervical herniated discs, on the other hand, may lead to shoulder and neck stiffness, radiating pain in the arms, or sensations of numbness. The specific location of the pain depends on the affected spinal region.
The disc is a cartilaginous and fibrous structure located between the vertebrae, functioning like a soft cushion. It is soft, smooth, elastic, and contains a large amount of water. Its primary function is to absorb and distribute the impact forces generated by daily activities such as walking, running, bending, and jumping. It effectively protects the vertebrae from damage due to friction or pressure.
The disc consists of an outer tough fibrous ring and a central gel-like nucleus. When the nucleus is subjected to excessive pressure, it can cause the fibrous ring to bulge outward or even rupture. If the nucleus protrudes through the ruptured fibrous ring and compresses nearby nerves, it results in what is known as a "herniated disc."
Is There a Difference Between Sciatica and Herniated Discs?
Sciatica is not the same as a herniated disc. There are many causes of sciatica, and a herniated disc is one of the more common ones. Sciatica is a symptom that refers to pain, numbness, or tingling caused by pressure or irritation of the sciatic nerve, usually extending from the buttocks down to the calf or foot. When a herniated disc compresses a nerve root or the spinal cord, it can lead to pain or discomfort. The range and severity of sciatica depend on the location and degree of nerve compression, which can be categorized into "bony compression" and "muscle compression." A herniated disc falls under "bony compression" and is one of the most common causes. Approximately 90% of sciatica cases are caused by lumbar disc herniation, particularly involving the fourth and fifth lumbar vertebrae (L4-L5) or the fifth lumbar and sacral vertebrae (L5-S1). When a herniated disc compresses the sciatic nerve root, it can trigger sciatica, resulting in typical radiating pain, sensory abnormalities, or muscle weakness.
How to Differentiate Between the Two?
- Sciatica: Pain along the pathway of the sciatic nerve, possibly accompanied by numbness, tingling, or muscle weakness.
- Herniated Disc: A specific structural issue that only causes sciatica symptoms (lower limb numbness/ pain) when it compresses a nerve.
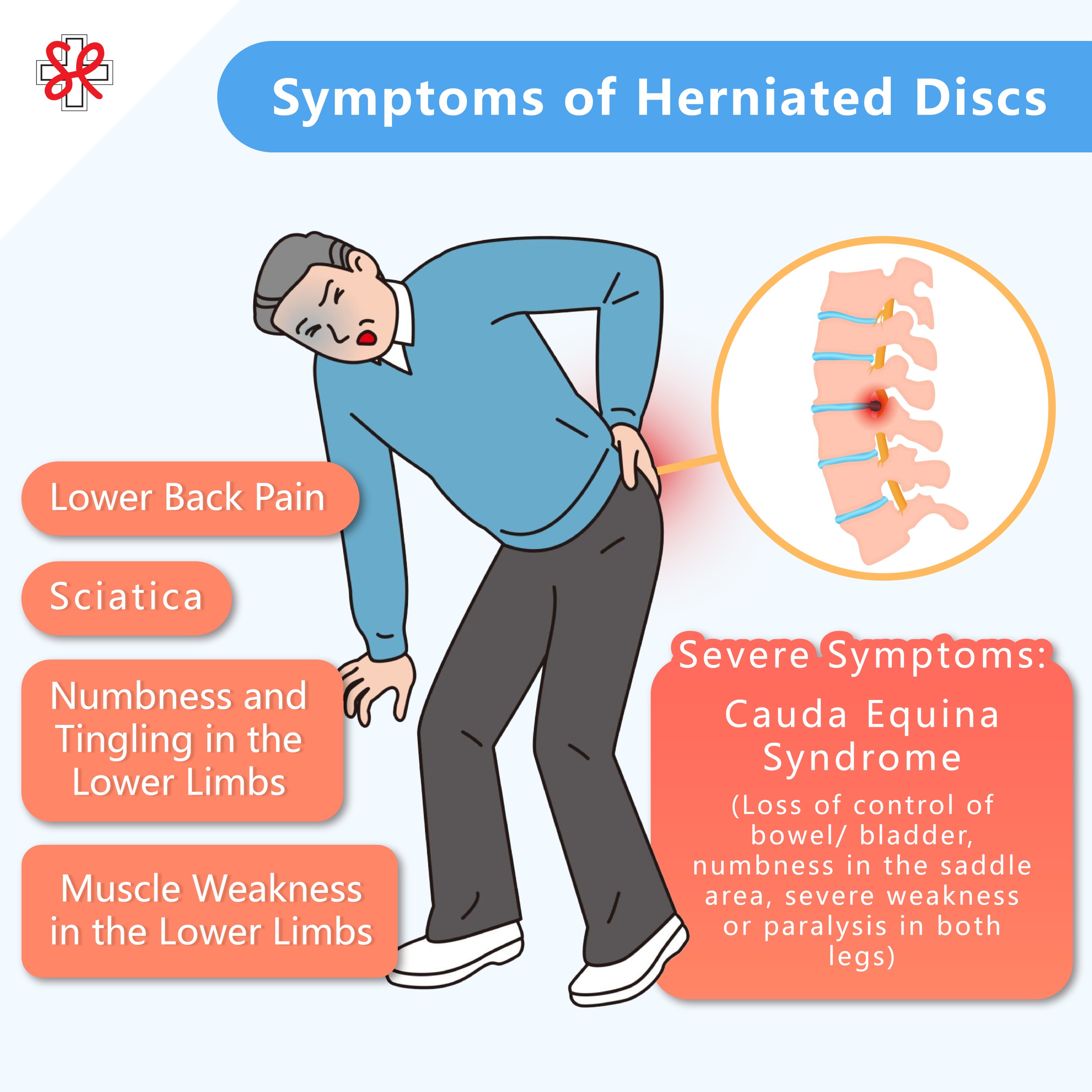
Symptoms of Herniated Discs
( ![]() Click the image to enlarge )
Click the image to enlarge )
A herniated disc can trigger different symptoms depending on the location of the herniation and the degree of nerve compression. Generally, symptoms can be categorized into chronic and acute types. Chronic herniated discs are often related to disc degeneration; since the condition lasts longer and the herniated portion does not typically compress nerve roots, it usually does not cause noticeable or severe symptoms. In contrast, acute herniated discs are often caused by sudden tears, and when the nucleus protrudes and compresses nerve roots, it can lead to more severe symptoms. Below are common symptom classifications:
Lower Back Pain
One of the most typical early symptoms of a herniated disc is lower back pain, particularly concentrated in the lower back or lumbar area. This pain can range from mild discomfort to severe pain, potentially affecting daily activities. The lower back may experience persistent or intermittent pain, especially exacerbated by coughing, sneezing, standing or sitting for prolonged periods, bending, or lifting heavy objects.
Sciatica
When the herniated disc compresses the sciatic nerve, patients may experience characteristic radiating pain that includes:
- Radiating Pain: Starting from the lower back, extending through the buttock and the back of the thigh down to the calf and even the sole of the foot, often described as an electric shock sensation.
- Worsening Condition: Pain intensifies during coughing, sneezing, or bending.
- Numbness and Weakness: The affected leg may feel numb, tingly, or even experience a reduction in muscle strength.
Numbness and Tingling in the Lower Limbs
If the disc compresses the nerve roots, patients may experience the following abnormal sensations:
- Numbness and Tingling: The legs or feet may feel numb, tingly, or have a burning sensation.
- Difficulty Walking: Some patients may feel unable to lift their feet normally while walking, leading to tripping.
- Abnormal Sensation: Some patients describe feelings like "pins and needles" or "burning," which are signs of nerve compression.
Muscle Weakness in the Lower Limbs
Compressed nerves can lead to decreased muscle strength in the legs, affecting stability while walking and the ability to climb stairs. Some patients may also feel that their legs fatigue easily, significantly reducing their activity levels.
Cauda Equina Syndrome (Severe Symptoms)
In rare cases, if the disc severely compresses the cauda equina nerves (a crucial bundle of nerves at the base of the spine), the following dangerous signals may occur:
- Loss of Control of Bowel or Bladder: Inability to control urination or defecation.
- Numbness in the Saddle Area: Numbness or loss of sensation in the area around the genitals and inner thighs.
- Severe Weakness or Paralysis in Both Legs: Significantly affecting the ability to walk.
Cauda equina syndrome is a medical emergency; if you experience related symptoms, seek immediate medical attention to prevent permanent nerve damage. If you exhibit any of the above symptoms, it is also advisable to seek medical examination as soon as possible to determine the cause and develop an appropriate treatment plan.
Acute vs. Chronic Herniated Discs: Differences in Symptoms and Management
The course of a herniated disc is typically classified into acute and chronic phases based on the duration and severity of symptoms. Understanding the distinctions between the two can help in selecting the most appropriate management strategy.
Rehabilitation and care after surgery for meniscal injuries and cruciate ligament tears differ slightly, primarily in terms of focus on knee joint stability and details of the recovery process.
| Feature | Acute Herniated Disc (Acute) | Chronic Herniated Disc (Chronic) |
| Definition (Time) | Shorter duration of symptoms, generally lasting from a few days to 6 weeks. | Longer duration of symptoms, typically lasting over 6 weeks or 3 months, or recurring. |
| Main Causes | Sudden trauma, bending to lift heavy objects, strains, etc., leading to a sudden rupture of the disc's fibrous ring. |
Poor posture over time, cumulative strain, and gradual degeneration of the disc structure. |
| Nature of Pain |
Intense, sharp, unbearable stabbing or burning pain, often accompanied by |
Persistent, intermittent dull pain or aching, with varying degrees of pain intensity. |
| Symptoms | May exhibit noticeable postural deformity (body tilt), severe muscle spasms, and numbness or radiating pain due to nerve compression. | May experience muscle weakness, limited range of motion (stiffness), and persistent nerve-related numbness that is hard to alleviate. |
| Activity Level | Severe pain leads to significant limitations in mobility, making it difficult to bend, rise, or walk. | Stiffness or persistent pain results in ongoing limitations in mobility, affecting daily life and exercise. |
| Management Methods | Rest, medication (anti-inflammatory pain relief), ice application to control severe pain and inflammation. | Physical therapy, core strengthening exercises, posture correction to rebuild spinal stability. |
| Rehabilitation Focus | Begin gentle stretching exercises once pain and inflammation subside | Continue to strengthen core muscles and lower limb strength to restore normal life and exercise functionality. |
| Common Surgical Methods | Minimally invasive decompression surgery | Minimally invasive decompression surgery or disc fusion surgery |
Causes and Risk Factors of Herniated Discs
The causes and risk factors for herniated discs include:
Common Causes
- Degenerative Changes: Aging is one of the primary causes of herniated discs. As we age, the discs gradually lose moisture and elasticity, causing the fibrous ring to become stiff and prone to rupture.
- Excessive Load: Certain occupations require repeated lifting, pushing, or bending, such as construction or moving jobs. Frequently lifting heavy objects with improper posture or using back muscles instead of leg strength can place excessive pressure on the spine, accelerating disc wear and leading to damage.
- Accidental Injury: External traumatic events like falls, impacts, or sprains can directly tear the fibrous ring of the disc.
Other Risk Factors
- Obesity: Being overweight or obese increases the pressure on the spine, accelerates disc degeneration, and raises the risk of herniation.
- Poor Posture: Maintaining poor posture over time, such as slouching, looking down at devices for extended periods, or incorrect sitting positions, can place excessive stress on the spine.
- Smoking: Smoking decreases the body’s ability to supply nutrients to the discs, accelerating degeneration and increasing the risk of herniation.
- Genetic Factors: Some individuals may be more prone to herniated discs due to hereditary factors.
- History of Back Pain: Individuals with a history of back injuries or chronic pain are more likely to experience recurring back issues, including pain caused by herniated discs.
- Prolonged Sitting or Standing: Maintaining prolonged sitting or standing positions can exert continuous pressure on the spine, increasing the likelihood of disc herniation.
How is a Herniated Disc Diagnosed?
If you suspect that you have symptoms related to a herniated disc, such as sciatica, leg numbness, or lower back pain, it is advisable to seek medical evaluation promptly. Typically, the doctor will first review your symptoms and medical history, followed by a physical examination and relevant tests to confirm the presence of a herniated disc. Here are common examination methods:
Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging (MRI) is a non-invasive imaging diagnostic technique that uses strong magnetic fields and radio waves to generate detailed images of internal structures in the body. MRI scans are particularly suitable for examining soft tissues, such as the spinal cord, nerve roots, intervertebral discs, muscles, and ligaments. The advantage of MRI lies in its ability to capture high-resolution cross-sectional images from multiple angles, allowing doctors to clearly observe the anatomical structures of the spine, accurately diagnose the location, size, and severity of the herniated disc, and assess the compression on surrounding nerve roots and the spinal cord. Compared to other imaging techniques, MRI provides higher resolution for soft tissues. Additionally, MRI can show the degree of disc degeneration and whether inflammation or other lesions are present.
X-ray Examination
X-rays are a commonly used imaging tool that can clearly display the skeletal structure of the spine but cannot show details of soft tissues. They are primarily used to rule out other potential causes of back pain, such as fractures, spinal displacement, or instability. However, in most acute cases of lumbar disc herniation, X-rays typically do not reveal clear abnormalities or specific changes.
Treatment Methods for Disc Herniation
The treatment methods for disc herniation are diverse, ranging from conservative approaches to surgical interventions. The choice of an appropriate treatment method depends on the severity of symptoms, the duration of the condition, and its impact on daily life. Here are the main treatment options:
Non-Surgical Treatment (Conservative Treatment)
Most patients with disc herniation do not require surgery; initial treatment typically involves non-surgical methods aimed at alleviating pain and promoting recovery.
1. Rest and Activity Adjustment
Short-term rest (1 to 2 days) can help relieve back and leg pain. It is recommended to avoid prolonged standing or sitting and to minimize large movements, such as bending and lifting heavy objects.
2. Medication
Medication is aimed at relieving pain and reducing inflammation. Commonly used medications include:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Used to reduce pain and inflammation.
- Muscle Relaxants: Help alleviate muscle spasms and tension.
- Neuropathic Pain Medications: Target and relieve nerve pain caused by nerve damage or compression.
3. Physiotherapy
Physiotherapy is an important part of recovery from a disc herniation. The main goals are to strengthen the muscles that support your spine, improve posture and flexibility, reduce pain, and help you return to your normal daily activities safely.
A physiotherapy program is carefully tailored to each person's condition and usually includes a combination of treatments designed to relieve pressure on the spine, improve mobility, and support healing.
Spinal Traction Therapy gently stretches the spine to reduce pressure on nerves and relieve discomfort.
Exercise Therapy focuses on strengthening your core and back muscles, improving flexibility, and helping you maintain good posture to protect your spine.
Heat or Ultrasound Therapy helps relax tight muscles, improve blood flow, and speed up tissue repair.
Electrical therapy, such as interferential or shockwave treatment, can help reduce inflammation, ease muscle tension, and relieve pain.
Through regular sessions and guided home exercises, physiotherapy helps manage symptoms, promote healing, and lower the risk of future injury.
The Rehabilitation Center at St. Paul's Hospital is managed by a team of professional physiotherapists, dedicated to creating personalized treatment plans for patients with disc herniation, including stretching exercises and stability training to help patients regain mobility and prevent re-injury. For professional rehabilitation services, please schedule an appointment with the Rehabilitation Center at St. Paul's Hospital.

Surgical Treatment
Surgical intervention may be considered when conservative treatments are ineffective or if neurological function continues to deteriorate.
1. Discectomy
Discectomy involves removing the protruding disc tissue to relieve pressure on the nerves. It can be performed via traditional open surgery or minimally invasive techniques:
- Traditional Open Surgery: Requires general anesthesia and involves an incision of about 8 to 10 centimeters in the lower back, removing bone from the vertebra and excising the protruding disc.
- Minimally Invasive Surgery: Conducted with precision equipment and high-definition optical lenses, with an incision of only about 1.6 centimeters. Specialized instruments are used to separate some muscle tissue, access the vertebra, and remove the affected disc with minimal trauma and faster recovery.
2. Fusion Surgery
This procedure involves fusing adjacent vertebrae together, suitable for patients with spinal instability or recurrent herniation.
Professional Advice and Follow-Up Services
Our orthopedic specialists at the Specialist Outpatient Department, St. Paul's Hospital are dedicated to providing diverse orthopaedic diagnosis and advanced minimally invasive surgical options for patients with disc herniation and various spinal and joint pain conditions. Doctors tailor personalized treatment plans based on patients' conditions, offering comprehensive follow-up from initial consultation, examination, surgery, to post-operative rehabilitation. If patients experience persistent nerve compression pain, mobility issues, or require further evaluation of treatment options, please schedule an appointment with our orthopedic specialist at St. Paul's Hospital.
Frequently Asked Questions
Does a Herniated Disc Require Additional Testing?
In addition to routine magnetic resonance imaging (MRI) and X-rays, doctors may recommend further testing based on the patient's specific situation, such as electromyography (EMG) and nerve conduction studies.
What Conditions May Arise After Surgery?
After lumbar disc surgery, most patients experience significant improvement in symptoms. However, a small number may initially experience numbness, tingling, limited range of motion, muscle tightness, or mild pain, which are generally part of the normal recovery process.
Currently, most surgeries are performed using minimally invasive techniques, allowing for quicker recovery and very low risk. However, patients should still avoid excessive weight-bearing and high-intensity activities and continue with appropriate stretching exercises. With progress in rehabilitation and regular follow-ups as advised by the doctor, these symptoms can gradually improve.
What Are the Risks of Surgery?
Risks associated with herniated disc surgery include:
- Infection: There may be an infection at the surgical site requiring antibiotic treatment.
- Recurrent Herniation: Some patients may experience a recurrence within a few years post-surgery.
- Persistent or Worsening Pain: The surgery may not completely alleviate symptoms.
- Nerve Damage: In very rare cases, this may lead to loss of sensation or muscle dysfunction.
- Bleeding and Spinal Instability: Possible complications during the surgical process.
- Anesthesia Risks and Other Complications: Such as pneumonia or blood clots.
Although the incidence of most complications is low, it is important to discuss personal health conditions and related risks thoroughly with the doctor before deciding on surgery.
Will a Herniated Disc Heal Naturally?
Most patients with mild to moderate herniated discs have a chance of experiencing improvement in pain over a few weeks to months with rest, gentle activity, and rehabilitation, without the need for surgery. However, if symptoms are severe or continue to worsen, it is advisable to seek medical evaluation promptly.
How can I avoid getting a Herniated Disc?
While herniated discs cannot be completely prevented, the following measures can effectively reduce the risk:
- Good Posture: Maintain a straight back whether standing or sitting, using a lumbar support cushion when seated.
- Avoid Prolonged Sitting or Standing: Get up and move every hour to alleviate back fatigue.
- Proper Lifting Techniques: Bend at the knees to squat down, using leg and hip strength to bear weight, keeping the natural curve of the lumbar spine without bending over.
- Suitable Sleep Products: Use a mattress and pillow that offer good support.
- Reduce Looking Down: Avoid prolonged periods of looking down at electronic devices to prevent increased spinal load, which can lead to herniation, inflammation, or even degeneration or bone spurs.
- Exercise Habits: Engage in core training to strengthen back muscles, ensuring to warm up adequately before exercising.
- Healthy Weight: Maintain a healthy weight to reduce pressure on the spine.
By following these methods, the likelihood of developing a herniated disc can be effectively reduced, promoting spinal health. If you experience any suspected symptoms, it is recommended to seek medical evaluation as soon as possible to establish an appropriate treatment plan.